Identifying Liver Cirrhosis Symptoms and Exploring Treatment Paths
Understanding Liver Cirrhosis and Its Causes
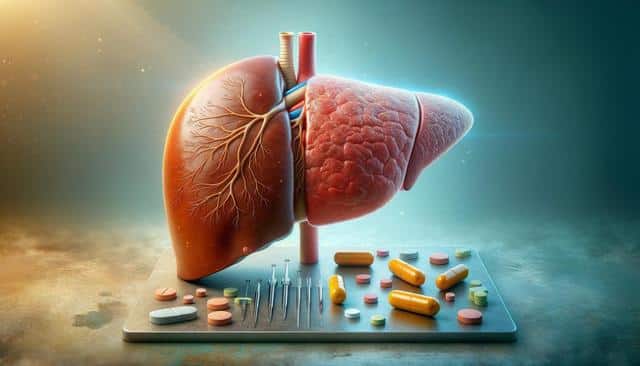
Liver cirrhosis is a progressive condition in which healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly. This scarring is often the result of long-term liver damage from chronic conditions. Common causes include chronic alcohol consumption, viral hepatitis (particularly hepatitis B and C), and nonalcoholic fatty liver disease. Over time, these conditions cause inflammation and cell death, leading to fibrosis and eventually cirrhosis.
The liver plays a crucial role in essential bodily functions such as detoxification, protein synthesis, and digestion. When it becomes damaged, these functions begin to decline, sometimes without noticeable symptoms in the early stages. This makes it particularly important to understand the risk factors and monitor liver health regularly, especially for individuals with preexisting liver conditions or those with a history of substance use.
Additional risk factors include:
- Obesity and metabolic syndrome
- Exposure to certain toxins or medications
- Genetic liver diseases such as hemochromatosis or Wilson’s disease
Identifying the underlying cause of liver damage is essential for tailoring appropriate treatment and slowing disease progression.
Recognizing Symptoms of Liver Cirrhosis
Symptoms of liver cirrhosis vary depending on the stage of the disease. In its early phase, cirrhosis may present with mild or non-specific symptoms, making early diagnosis challenging. As the disease progresses, more noticeable signs begin to appear, often indicating significant liver impairment.
Some of the early and advanced symptoms include:
- Fatigue and weakness
- Loss of appetite and unexplained weight loss
- Nausea and abdominal discomfort
- Jaundice (yellowing of the skin and eyes)
- Swelling in the legs, ankles, or abdomen (ascites)
- Itchy skin and easy bruising
In more advanced stages, complications such as hepatic encephalopathy (mental confusion due to liver toxin buildup), internal bleeding from varices, and liver cancer may develop. Monitoring these symptoms and seeking medical advice promptly can improve outcomes significantly.
Diagnostic Methods and Tests
Diagnosing liver cirrhosis involves a combination of physical examinations, laboratory tests, and imaging studies. Physicians typically begin with a review of the patient’s medical history and an assessment of risk factors. Blood tests can indicate liver function by measuring levels of enzymes, bilirubin, and proteins such as albumin.
Common diagnostic tools include:
- Liver function tests (LFTs)
- Complete blood count (CBC) and coagulation panels
- Ultrasound or CT scan of the abdomen
- Transient elastography (FibroScan) to measure liver stiffness
- Liver biopsy when necessary for confirmation
These tests help determine the extent of liver damage and rule out other potential causes of symptoms. Early diagnosis through regular check-ups is particularly important for individuals at higher risk of liver disease. Medical professionals may also screen for related complications, such as portal hypertension or esophageal varices, to adjust treatment plans accordingly.
Treatment Options for Liver Cirrhosis
While liver cirrhosis is generally not reversible, its progression can often be slowed or managed effectively with the right treatment approach. The primary goal of treatment is to address the underlying cause and prevent further damage to liver tissue. In addition, managing symptoms and complications is crucial for maintaining quality of life.
Standard treatment options include:
- Antiviral medications for hepatitis B or C
- Lifestyle changes, including alcohol cessation and dietary adjustments
- Weight loss and control of blood sugar in cases of nonalcoholic fatty liver disease
- Diuretics for fluid retention and medications to reduce portal pressure
- Endoscopic procedures for bleeding varices
In severe cases where liver function is significantly impaired, a liver transplant may be considered. This procedure involves replacing the damaged liver with a healthy donor organ and is typically reserved for individuals meeting specific medical criteria. Post-transplant care includes lifelong immunosuppressive therapy and regular monitoring.
Working closely with a hepatologist or liver specialist helps ensure a personalized treatment strategy that aligns with the patient’s specific condition and health status.
Lifestyle Considerations and Long-Term Management
Managing liver cirrhosis often requires long-term lifestyle adjustments and ongoing medical supervision. Individuals diagnosed with the condition are encouraged to make proactive choices that support liver health and reduce strain on the organ. This includes avoiding alcohol and over-the-counter medications that may be toxic to the liver, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
Key lifestyle measures include:
- Following a low-sodium diet to prevent fluid retention
- Ensuring adequate protein intake to maintain muscle mass
- Receiving vaccinations for hepatitis A and B, as well as influenza and pneumococcal infections
- Attending regular follow-up appointments for liver function monitoring
- Engaging in physical activity tailored to one’s ability and overall health
Mental health support is also a crucial component of long-term care, as chronic illness can significantly impact emotional well-being. Support groups, counseling, and education about the condition can empower individuals and caregivers to manage the disease more effectively. With proper care and vigilance, many people with liver cirrhosis can maintain a functional and fulfilling lifestyle.
Conclusion: Taking Action for Liver Health
Liver cirrhosis is a serious condition that requires timely recognition, accurate diagnosis, and a comprehensive treatment approach. Understanding the symptoms, risk factors, and available medical interventions is essential for effective disease management. Whether you’re personally affected or supporting someone with liver cirrhosis, staying informed and working closely with healthcare providers can make a significant difference. Prioritizing liver health through lifestyle choices and regular check-ups is one of the most proactive steps toward improving long-term outcomes.


