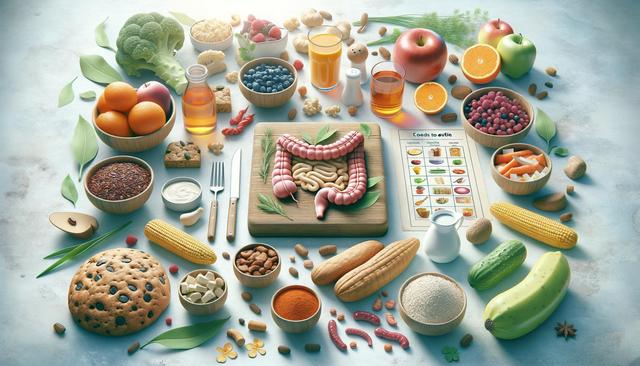
A Guide to Identifying Foods to Avoid with Ulcerative Colitis
Learn which foods to avoid if you have ulcerative colitis. This guide explains dietary triggers, offers meal planning tips, and supports symptom management through smart eating choices that may reduce inflammation and improve digestive health long-term.
Understanding Ulcerative Colitis and the Role of Diet
Ulcerative colitis is a chronic inflammatory condition of the colon and rectum that can significantly affect daily life. While there is no one-size-fits-all diet for everyone with this condition, identifying and avoiding certain foods can help reduce flare-ups and support overall digestive health. Since ulcerative colitis affects the lining of the colon, foods that irritate or stimulate the gut excessively are often problematic. It’s important to understand that dietary triggers can vary from person to person, so keeping a food diary and working with a healthcare provider or dietitian can be especially helpful.
Diet plays a supportive role in managing symptoms like abdominal pain, diarrhea, and fatigue. When inflammation is active, the gut becomes more sensitive to specific food components. Many people with ulcerative colitis find relief by avoiding foods that are hard to digest, promote gas, or are known to be inflammatory. Making informed food choices is a proactive way to support medical treatment and improve quality of life over time.
Common Food Triggers to Avoid
Some foods are frequently reported to trigger symptoms in individuals with ulcerative colitis. While reactions can differ, there are several categories of food that many people find problematic:
- Dairy products: Those who are lactose intolerant may experience worsened symptoms from milk, cheese, and other dairy-based items.
- High-fiber foods: Raw vegetables, whole grains, and legumes can be too rough on the digestive tract during flare-ups.
- Spicy foods: Ingredients like hot peppers and chili powder may irritate the lining of the colon.
- Fatty or fried foods: These can be difficult to digest and may lead to diarrhea or cramping.
- Caffeinated beverages: Coffee, tea, and energy drinks may stimulate the bowels and contribute to urgency or discomfort.
Each person’s experience is unique, so identifying personal triggers through trial and error, while maintaining a balanced diet, is essential. Eliminating these common irritants may help calm inflammation and support remission periods.
Processed Foods and Additives
Processed foods often contain ingredients that may not be well tolerated by individuals with ulcerative colitis. These include preservatives, emulsifiers, and artificial sweeteners, which can disrupt gut bacteria and potentially worsen symptoms. Foods high in added sugars or refined carbohydrates may also contribute to inflammation and should be limited when possible.
Some examples of processed foods to approach with caution include:
- Packaged snacks like chips and crackers
- Frozen meals with long ingredient lists
- Sugary breakfast cereals
- Soda and sweetened drinks
- Fast food and takeout meals
Reading nutrition labels carefully and opting for whole, minimally processed foods can help support digestive health. Preparing meals at home allows for better control over ingredients and can reduce exposure to potential irritants.
Tips for Safer Meal Planning
Managing ulcerative colitis through diet involves more than just avoiding certain foods. Meal planning with a focus on gentler ingredients and appropriate cooking methods can go a long way in maintaining symptom control. During flare-ups, soft, bland foods are often better tolerated, while remission periods may allow for a broader range of options.
Consider these tips when planning meals:
- Choose low-residue foods that are easier to digest, such as white rice, bananas, and cooked carrots
- Use cooking methods like steaming, baking, or boiling instead of frying
- Eat smaller, more frequent meals to reduce stress on the digestive system
- Stay hydrated with water, herbal teas, or electrolyte-rich drinks
- Introduce new foods one at a time to monitor tolerance
Keeping a food and symptom journal can help identify patterns and guide future choices. It’s also useful to work with a registered dietitian who understands inflammatory bowel diseases and can help tailor a plan that meets nutritional needs without aggravating symptoms.
When to Seek Professional Guidance
While dietary adjustments can make a noticeable difference in managing ulcerative colitis, they should complement—not replace—medical treatment. If symptoms persist despite dietary changes, or if you experience significant weight loss, fatigue, or nutrient deficiencies, it’s important to consult a healthcare provider. They may refer you to a dietitian who can assess your current intake and recommend strategies to restore balance.
In some cases, additional testing may reveal food sensitivities or deficiencies that need targeted interventions. Nutritional supplements might also be necessary, especially during periods of active inflammation when absorption is impaired. A professional can help ensure that your diet supports your overall treatment plan and long-term health goals.
Ultimately, managing ulcerative colitis through diet is a dynamic process. What works well during one phase may need to be adjusted later. Staying informed, flexible, and proactive can make a meaningful difference in how you feel day to day.
Conclusion: Supporting Digestive Health with Informed Choices
Living with ulcerative colitis requires a thoughtful approach to food and nutrition. While trigger foods vary from person to person, avoiding common irritants like high-fiber raw vegetables, spicy dishes, and processed snacks can help reduce flare-ups. Incorporating gentle cooking techniques and safer meal options can support digestion and contribute to overall well-being. By staying attentive to your body’s responses and seeking professional guidance when needed, you can develop a sustainable and nourishing dietary routine that complements your treatment and enhances quality of life.